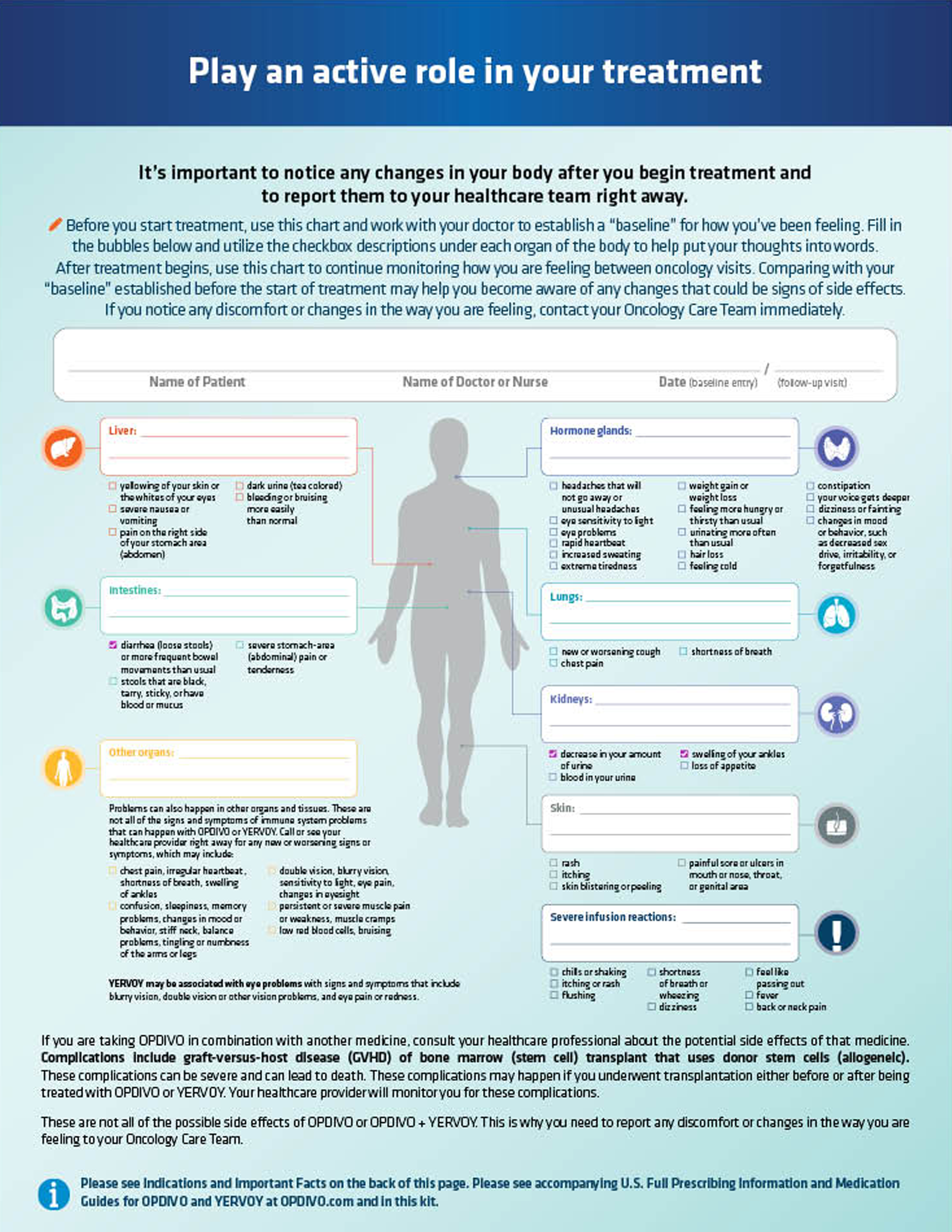
Patient Monitoring Checklist

Use this tool to help you document any noticeable changes or potential side effects during your course of treatment, then download the PDF and share it with your doctor.
Use this tool to help you document any noticeable changes or potential side effects during your course of treatment, then download the PDF and share it with your doctor.
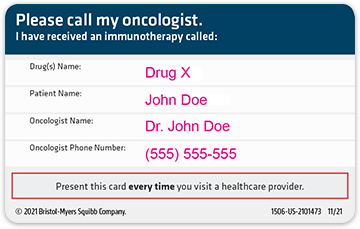
Patient Wallet Card

To keep your treatment and oncologist information close by, create a contact
card for future reference. This card can
be printed out or saved digitally to your device for easy access.
To keep your treatment and oncologist information close by, create a contact
card for future reference. This card can
be printed out or saved digitally to your device for easy access.
After completing the form below, download a PDF with your selections to share with your healthcare provider. This list does not include all side effects you could experience during treatment. Contact your doctor right away if you notice any changes or discomfort, along with new or worsening symptoms.
Please check all of the symptoms you are experiencing.
Lungs
Intestines
Liver
Hormone glands
Kidneys
Skin
Other organs
Problems can also happen in other organs and tissues. These are not all of the signs and symptoms of immune system problems that can happen with OPDIVO or YERVOY. Call or see your healthcare provider right away for any new or worsening signs or symptoms, which may include:
Severe infusion reactions
YERVOY may be associated with eye problems
with signs and symptoms that include:
If you are taking OPDIVO in combination with another medicine, consult your healthcare professional about the potential side effects of that medicine.
Complications, including graft-versus-host disease (GVHD), of bone marrow (stem cell) transplant that uses donor stem cells (allogeneic). These complications can be severe and can lead to death. These complications may happen if you underwent transplantation either before or after being treated with OPDIVO or YERVOY. Your healthcare provider will monitor you for these complications.
Contact your doctor right away if you notice any changes or discomfort, along with new or worsening symptoms.
Information collected on this form is for your use only and will not be saved or transmitted.
After you complete the form below, you can choose to download a PDF of the card and/or save it directly
to your contacts.
*Required fields
and will not be saved or transmitted.
THE OPDIVO + YERVOY
Side Effect Tracker

Keep track of symptoms and other important information so that you can proactively manage potential side effects with your doctor.
Download PDF
Keep track of symptoms and other important information so that you can proactively manage potential side effects with your doctor.
OPDIVO Treatment Journal

This treatment journal can help keep
track of side effects, important
information, and a list of current medications.
Download PDF
This treatment journal can help keep
track of side effects, important
information, and a list of current medications.
Questions to Ask
Your
Doctor
Here are some questions you may want to consider asking your healthcare provider about OPDIVO or OPDIVO + YERVOY
If you or a loved one are talking with a doctor about possible treatment options and you’re considering either an OPDIVO or an OPDIVO + YERVOY treatment, this can be a valuable tool to help you start a conversation with your doctor.
- What is immunotherapy?
- How is OPDIVO or OPDIVO + YERVOY different from traditional chemotherapy?
- How does OPDIVO or OPDIVO + YERVOY work?
- What are the potential benefits of an OPDIVO treatment?
- How are OPDIVO treatments given?
- How often will I need OPDIVO treatments and how long will they take?
- What are the potential side effects that I may experience?
- Will this treatment affect my daily life in any way?
- How will I know if the treatment is working?
When you are having a conversation with your doctor:
- Ask them to explain all the answers clearly to be able to make an informed decision
- You may want to take notes that you can refer to later
If you and your doctor are considering OPDIVO or OPDIVO + YERVOY be
sure to discuss your existing health problems, prescription
medications, and
Your doctor is always the best source of information when it comes to your health.



















 Download PDF
Download PDF